Adhesive Capsulitis, or “Frozen Shoulder” is a pathological process that is characterized by the progression and resolution of shoulder pain and mobility limitations. The entire process can last from 12-18 months. This specific pathology affects approximately 2-5% of the general population, but you may be at an increased risk if you have Diabetes (Type I or II), Thyroid disease, have a history of frozen shoulder on the opposite side, are between the ages of 40-65 years old or are female.
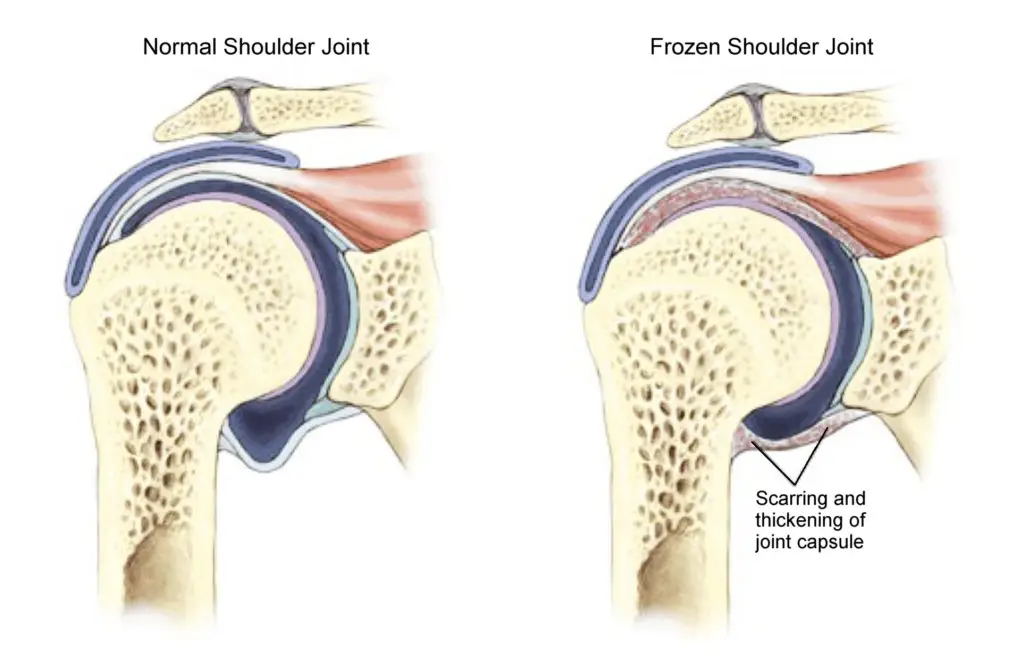
Adhesive Capsulitis begins with high levels of inflammation in the shoulder joint that lead to the thickening and contracture of the ligaments and tendons that surround the joint. Researchers have seen new growth of blood vessels and nerves in these structures that may help explain why this can be so painful for patients. The cause of this pathology isn’t well understood; it can occur after a trauma to the shoulder, be it surgery or an injury, but also with no significant history of trauma. No matter the cause, most patients see a full recovery, while some report long-term issues with shoulder pain and stiffness. The disease process can be loosely classified into 4 different stages:
Stage | Symptoms | Duration |
Stage I, Initial Onset | Sharp end-range pain, achy at rest, disturbed sleep | 0-3 months |
Stage 2, “Freezing” or “Painful” | Gradual loss of shoulder motion in all planes | 3-9 months |
Stage 3, “Frozen” | Continued pain and loss of motion | 9-15 months |
Stage 4, “Thawing” | Resolving pain and stiffness | 15-24 months |
So, what do we do about it?
Your physical therapist will perform a thorough evaluation of your medical history, your activity history and physical presentation. He or she will evaluate your pain levels, range of motion, muscle strength, joint mobility, neurological function and functional limitations based on your symptoms. Physical therapy treatment will then be driven by the patient’s level of irritability and may take place in multiple sessions over the course of the next year, due to the long disease process
In the initial stages, managing pain and inflammation are the top priority. Operative studies show that the initial stages of frozen shoulder include increased inflammation in the shoulder joint, but no adhesions or ligamentous changes. This may be the best time to trial corticosteroid injections, which may provide short-term relief, along with joint stretching and mobility exercises, during high irritability stages.
During the freezing stage, patients continue to experience high pain levels and a gradual loss of range of motion in the shoulder. At this point, operative findings now show increased inflammation in the joint, growth of new blood vessels and nerve endings and some loss of motion under anesthesia, which would indicate stiffening of the shoulder structures. At this point, your physical therapist will continue to monitor your pain levels as they continue to stretch and mobilize your affected shoulder without causing any significant increase in pain. Stretching and joint mobilizations can help to maintain capsular mobility and decrease pain and stiffness.
When the shoulder is “frozen”, the patient continues to report less pain, but has a significant loss in range of motion. The inflammation has continued to decrease, but the ligaments in the shoulder have also continued to thicken and stiffen and there is a significant loss of range of motion under anesthesia. Continued stretching and joint mobility exercises are important to maximize a patient’s functional range of motion at this stage.
Finally, the thawing stage shows a continued decrease in joint inflammation and a slow resolution in joint stiffness. The shoulder capsule has remained thickened and stiff, but will slowly loosen up with active and passive shoulder mobility. A patient should notice gradual improvement in their functional mobility with tasks like dressing, grooming, and reaching away from their body. These functional improvements can be increased dramatically with skilled physical therapy interventions to improve both the mobility of the joint and the strength of the surrounding muscles.
When diagnosed with Adhesive Capsulitis, it is important to understand the disease process. Because it can take a year or more to fully resolve, patients can get very discouraged with the progress of their shoulder throughout the rehab process and understanding your prognosis can help manage your expectations for your shoulder and how you may be affected by it. It is important to find a care team and a physical therapist who can guide and encourage you throughout your rehab, even when progress feels nonexistent.